Low Bone Density: Osteopenia and Osteoporosis
What is Osteopenia?
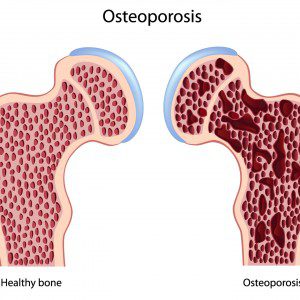
Osteopenia is a condition where your bone mineral density is lower than normal, but not yet severe enough to be classified as osteoporosis.
What is Osteoporosis?
Osteoporosis is also a condition of low bone mineral density but is more severe than osteopenia. Your risk of broken bones or fracture is increased. Primary osteoporosis occurs most often in postmenopausal women. Secondary osteoporosis occurs in anyone of any age as a result of chronic medical problems or secondary to prolonged use of medications, such as prednisone or antacids (proton pump inhibitors/PPI’s).
What causes osteoporosis? What causes osteopenia?
Bone density can be decreased by a number of factors including:
- Lack of Physical Activity/Exercise
- High stress
- Hormone imbalance
- Poor diet
- Smoking
- Excessive Alcohol Intake
- Vitamin D and/or vitamin K deficiency
- Soft drink intake
- Exposure to heavy metals like lead and cadmium
What is the natural treatment for Osteopenia/Osteoporosis?
Our naturopathic doctor emphasizes:
- lifestyle changes like regular physical activity and stress reduction techniques
- hormone balance through proper diet, and vitamins and herbs if necessary
- healthy diet – increasing foods that are beneficial to bone health and reducing foods that are detrimental
- changing unhealthy habits like smoking, alcohol abuse and soft drink intake
- testing for vitamin D or vitamin K deficiency and healthy supplementation if necessary (Note: patients on blood thinner medications are not advised to increase vitamin K intake)
- testing for heavy metal exposure and heavy metal detoxification if indicated
By Dr. Pamela Frank, Naturopathic Doctor, updated March 23, 2025
Research on natural treatment for osteopenia & osteoporosis
Diet:
A nutrient-rich diet full of calcium, phosphorus, iron, vitamins C and E, B vitamins, proteins, and unsaturated fats was associated with a 19% decrease in risk of wrist fractures and a 14% decrease in risk of fractures at any site. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Corticosteroid use and high intake of animal proteins and fats are negatively associated with bone loss while adhering to a vegan diet did not have adverse effects on bone loss and fracture. Source: Eur J Clin Nutr, 2011 Aug 3.
Curcumin:
Riva A, Togni S, Giacomelli L, Franceschi F, Eggenhoffner R, Feragalli B, Belcaro G, Cacchio M, Shu H, Dugall M. Effects of a curcumin-based supplementation in asymptomatic subjects with low bone density: a preliminary 24-week supplement study. Eur Rev Med Pharmacol Sci. 2017;
21(7):1684-1689.
● Bone density of the heel significantly improved in the curcumin supplementation group compared with baseline values; bone densities of small finger and jaw also improved significantly. No significant changes in bone density were observed in the control group.
Tea Drinkers:
Wu CH, Yang YC, Yao WJ, Lu FH, Wu JS, Chang CJ. Epidemiological evidence of increased bone mineral density in habitual tea drinkers. Arch Intern Med. 2002; 162(9):1001-6.
● Epidemiologic study finds habitual tea drinkers had greater lumbar spine bone mineral density compared with non-habitual green tea drinkers. Those with more than 10 years of green tea habitual consumption showed the highest bone mineral densities of all measured regions of the body.
Vitamin K2:
Vitamin K2 was found to boost bone health by increasing bone mineral density in osteoporosis patients and by decreasing incidences of fractures. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
New research suggests that vitamin K supplementation plus calcium and vitamin D can be beneficial to bone health. Source: J Korean Med Sci. 2011 Aug;26(8):1093-8.
Low-dose vitamin K2 supplementation in postmenopausal women was found to improve bone quality over 6-12 months. Source: J Bone Miner Metab, 2013 May 24.
Minerals:
In addition to calcium, magnesium, vitamin A and vitamin K all play a part in maintaining bone strength and flexibility. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Vitamin A:
Vitamin A was found to boost bone health by positively affecting osteoblast and osteoclast activity for proper bone remodeling. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Magnesium:
Magnesium must be present in the body in order for vitamin D and calcium to perform their jobs, therefore a deficiency can lead to osteoporosis. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Omega-3s:
Long-term aerobic exercise training plus omega-3 supplementation has a positive effect in reducing inflammation and augmenting BMD in postmenopausal osteoporosis. Source: Nutrition and Metabolism, Volume 8, page 71, 2011
Omega-3 fatty acid supplementation in addition to long-term aerobic exercise has a synergistic effect at reducing inflammation and augmenting bone mineral density in postmenopausal osteoporosis. Source: Nutr Metab (Lond). 2011; 8: 71.
Folic Acid:
Mice supplemented with folic acid for 6 weeks saw an improvement in blood flow to the bone and bone density. Source: J Orthop Res. 2011 Apr 5.
Calcium:
Adequate calcium and vitamin D throughout life may reduce the risk of osteoporosis. Source: Nutrition Research and Practice, Volume 5, Issue 1, pages 3-10, February 2011.
Supplementation with 800 mg/day of calcium and 400 IU/day of vitamin D3 was found to benefit bone health in female identical twins aged 9-13. Source: Osteoporos Int, 2010 June 11.
Supplementation with calcium combined with vitamin D was found to help prevent bone disease in children with renal diseases treated with steroids. Source: Nephrol Dial Transplant, 2013 May 2.
Lycopene:
Supplementation with lycopene-rich tomato juice or tomato Lyc-O-Mato lycopene capsules was found to significantly reduce oxidative stress and improve bone health in post-menopausal women. Source: Osteoporos Int, 2010 June 15.
Vitamin C:
Supplementation with 1000 mg/d vitamin C and 400 IU/d vitamin E may be useful in preventing or aiding in the treatment of aid-related osteoporosis. Source: J Nutr Health Aging, 2010; 14(6): 467-72.
Vitamin D:
Combined supplementation of calcium and vitamin D3 was effective in reducing the rate of bone mineral density loss in women with moderate chronic kidney disease. Source: Clin Nephrol, 2012 May; 77(5):358-65.
Vitamin D levels of 30 ng/ml may be required for bisphosphonate treatment in postmenopausal osteoporosis. Source: Bone. 2012 Apr 1.
Low vitamin D levels were found to be associated with an increased risk of stress fractures of the tibia or fibula. Source: J Bone Miner Res, 2011 June 22.
Qigong:
Qigong, a Chinese therapy close to Tai Chi involving movement and coordinated breathing patterns, was found to have a positive effect on bone density. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Potassium citrate:
Daily supplementation with potassium citrate, calcium, and vitamin D for 2 years led to a significant increase in areal bone mineral density and volumetric bone mineral density in elderly adults. Source: J Clin Endocrinol Metab. 2013 Jan;98(1):207-17.
Tocotrienol:
Treatment with delta-tocotrienol with lovastatin was found to significantly increase bone formation and reduce bone resorption in female rats. Source: Evidence-Based Complementary and Alternative Medicine, 2012.
Copper:
Copper supplementation may reduce oxidative stress and improve cross-linking of collagen in bone. Source: J Trace Elem Med Biol, 2010; 24(3): 165-8.
Green Tea:
A recent study found that green tea and tai chi reduce oxidative stress in postmenopausal women with osteopenia. Source: Complementary Prescriptions Journal, Vol.27, Issue 3, Feb 2013.
Green tea polyphenols and a regimen of Tai Chi were found to increase bone formation biomarkers, improve bone turnover rate, and improve muscle strength in osteopenic women. Source: Osteoporos Int, 2011 July 16.